Клинический случай описывает кровотечение язычной артерии как осложнение операции дентальной имплантации во фронтальном участке нижней челюсти.
How the simplest dental implant procedure can trigger an extremely serious complication
Giovanni Felisati1, Alberto Maria Saibene1, Daniele Di Pasquale1, Roberto Borloni2
+ Author Affiliations
1Department of Otolaryngology, San Paolo Hospital, University of Milan, Milan, Italy
2Department of Maxillofacial Surgery, Istituto Stomatologico Italiano, Milan, Italy
Correspondence to
Dr Giovanni Felisati, giovanni.felisati@gmail.com
Summary
A 62-year-old man came to our attention after an operation in a small dental outpatient clinic where only a single dentist was working. The man was showing complications after insertion of a dental implant in the anterior segments of the mandible. Bleeding led to a slow swelling of the neck with airway obstruction. Only an immediate intervention by a mobile emergency unit and prompt tracheal intubation avoided death by asphyxia. The patient was then transferred to our hospital. We inspected the patient and we performed a CT scan that showed complete airway obstruction. First, we performed a tracheotomy in order to ensure the airway patency and then we identified the source of bleeding: the mylohyoid artery placed anomalously close to the mandible. After clamping and tying the artery, the bleeding resolved. One day after the procedure, the tracheotomy was closed; the patient was discharged after 3 days.
Background
This case shows that even simple implantological procedures, often considered routine and risk-free, can lead to severe and potentially lethal complications. Oral surgeons and dentists, no matter how skilled and experienced in implantological surgery, must be at all times aware of this kind of complication, in order to promptly plan an emergency intervention. Careful attention must be paid not only during surgery, but also in the postoperative period. This is especially true for dentists, particularly those working in small outpatient clinics: dentists often cannot treat and solve their own complications. As a general rule, in our opinion, any kind of surgery, even the simplest procedure, must be performed by at least two surgeons.
Case presentation
A 62-year-old man came to our attention showing complications resulting from a single dental implant placement in the anterior third of the mandible (incisor region 42). The dental implant surgery was performed by an experienced dentist in his own outpatient clinic, under local anaesthesia. During the procedure, the dentist did not encounter any surgical problem and completed the implant placement. After the procedure, he did not notice any apparent problem and he asked the patient to stay in the waiting room for a standard period of observation. Submucosal bleeding and consequent slow swelling of the floor of the mouth followed implant placement. The dentist tried to solve the problem by removing the implant, but he noticed only a very limited haemorrhage from the dental alveolus. The submucosal bleeding continued, supplying a lingual, sublingual, submandibular and submental haematoma that displaced the tongue and floor of the mouth and led to airway obstruction. The immediate intervention of a mobile emergency unit who performed a prompt tracheal intubation prevented death by asphyxia. The patient was then transferred to our hospital and arrived there sedated, with assisted respiration via the nasotracheal tube.
Investigations
The physical examination reported diffuse haematoma under the mucosa of the floor of the mouth which displaced the tongue cranially
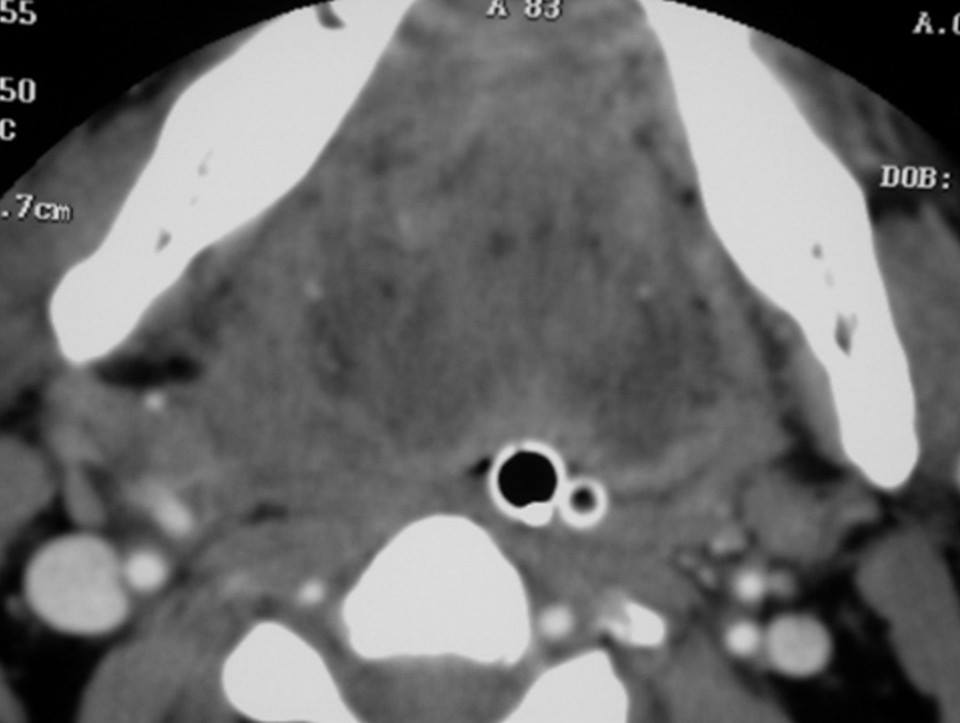
Figure 1. Axial CT image showing complete airway obstruction; the nasotracheal and the nasogastric tubes are completely surrounded by soft tissue swelling.
A CT scan was immediately performed and showed complete airway closure. The nasotracheal tube and the nasogastric tube were completely and tightly surrounded by the haemorrhagic and oedematous tissues of the base of the tongue and the neck.
Figure 2. Sublingual haematoma as observed after tracheotomy and before surgery; the nasotracheal tube has already been removed.
No other imaging examinations (such as three-dimensional MR angiography which would have been useful in locating the source of bleeding) were performed due to the urgency of performing tracheostomy and blocking haemorrhage in order to avoid the risk of accidentally moving the tube (considering that a new tube insertion would not have been possible).
Treatment
First, we chose to perform a tracheotomy, in order to grant airway patency for ventilation. Second, we performed an incision of the mucosa on the lingual gingival margin, from canine to canine (33–43), raising a mucosal flap. We identified the source of bleeding: an artery, close to the jaw, that we clamped and tied. The artery was found in an anomalous position. The dentist injured the arteriovenous lingual plexus, more specifically, an artery we identified as the mylohyoid artery. We did not find any alteration of the bony profile of the anterior segments of the mandible. We, therefore, cannot clearly establish the cause of the arterial injury. Tying of the artery and evacuation of the haematoma led to resolution of the clinical problem. The tracheotomy tube was retained for 1 day for safety purposes (figure 3). One day after the procedure, the tracheotomy tube was removed and the tracheotomy was closed surgically. After 3 days, the patient was discharged in good condition, his neck swelling almost completely reabsorbed.
Figure 3. Ventilation of the patient the day after surgery, before removal of the tracheotomy tube.
Outcome and follow-up
The patient underwent ear, nose and throat follow-up at 7, 30 and 60 days, showing complete reabsorption of the haematoma (figure 4). Prompt tracheal intubation prevented any neurological hypoxic sequelae. The patient successfully underwent another implantological procedure 6 months later in an inpatient clinic.
Figure 4. Seven days follow up; in the photo, we can appreciate a considerable reabsorption of the haematoma.
Discussion
The insertion of endosseous dental implants, or even more invasive preimplantological procedures such as maxillary sinus floor augmentation, are presently considered as safe and reliable techniques.1–3 Nevertheless, the wide diffusion and the sheer large number of these procedures inevitably leads to significant complications. It is worth pointing out that in Italy alone every year more than 1.5 million dental implants are sold.
Some exceptional cases of haemorrhage under the mucosa related to dental implantation in the frontal jaw are reported.4–7 These complications are uncommon at best, and dentists tend to underestimate the problem. The dental surgeon should never forget to address the patient with a complete informed consent.
In our reported case, the dentist, although well experienced, did not notice any anomaly or signs of ongoing complications, though he managed the complication well: a long postoperative observation period coupled with the prompt request for an emergency intervention saved the patient’s life. During our treatment, we observed the injured artery, though the overlying mucosa and close cortical bone were intact: we could discard direct damage and detachment of bone splinters as cause of the injury. Therefore, damage to the artery remains unexplained and we have to assume that it occurred while raising the flap on the lingual margin or after detachment of a tiny bone splinter which had not been discovered during subsequent surgery.
As reported in the literature, haemorrhage may start immediately or with some delay after vascular injury. In the reported case, no immediate bleeding was apparent: we, therefore, stress the importance of an observation period after surgery which should last at least 1 h.
The removal of the implant is the first procedure to perform in case of a submucosal haemorrhage, even if in this case, it was not enough to reduce or solve bleeding, haematoma and related dyspnoea.
Some authors recommend the use of short implants in the inferior frontal mandibular region in order to prevent the bleeding complications described in this article.5
Although no reports of death secondary to sublingual haematoma formation have been published, it is a potentially life-threatening complication.6
When treating potentially life-threatening swelling of the floor of the mouth, our choice, as previously reported, is to perform a tracheotomy first. A tracheotomy grants ventilation of the patient in case of occasional displacement or complete removal of the nasotracheal tube during surgery or in the postoperative period. As a matter of fact, considering the massive airway obstruction shown by the CT scan, a reintubation of the patient would have been impossible.
Learning points
Any surgical procedure can lead to serious complications.
Even in ‘small’ dental procedures a careful and adequate postoperative observation is mandatory.
Never delay an emergency unit intervention in case of potential airway obstruction.
If the airway obstruction is massive, tracheotomy is needed even when the patient already has a nasotracheal tube in place.
As a general rule, any kind of surgery, even outpatient dental surgery, should be performed by at least two surgeons.
Footnotes
Competing interests None.
Patient consent Obtained.
References
↵ Chiapasco M, Felisati G, Maccari A, et al. The management of complications following displacement of oral implants in the paranasal sinuses: a multicenter clinical report and proposed treatment protocols. Int J Oral Maxillofac Surg 2009;38:1273–8. [CrossRef][Medline]Google Scholar
↵ Colletti G, Felisati G, Biglioli F, et al. Maxillary reconstruction and placement of dental implants after treatment of a maxillary sinus fungus ball. Int J Oral Maxillofac Implants 2010;25:1041–4. [Medline][Web of Science]Google Scholar
↵ Chiapasco M, Felisati G, Zaniboni M, et al. The treatment of sinusitis following maxillary sinus grafting with the association of functional endoscopic sinus surgery (FESS) and an intra-oral approach. Clin Oral Implants Res Published Online First: 8 March 2012. doi: 10.1111/j.1600-0501.2012.02440.x.. Google Scholar
↵ Laboda G. Life-threateninig hemorrhage after pleacement of an oral endeosseous implant. Report of a case. J Am Dent Assoc 1990;121:599–600. [Abstract]
↵ Givol N, Chaushu G, Halamish-Shani T, et al. Emergency tracheostomy following life-threatening hemorrhage in the floor of the mouth during immediate implant placement in the mandibular canine region. J Periodontol 2000;71:1893–5. [CrossRef][Medline][Web of Science]Google Scholar
↵ Isaacson TJ. Sublingual hematoma formation during immediate placement of mandibular endosseous implants. J Am Dent Assoc 2004;135:168–72. [Abstract/FREE Full text]
↵ Kalpidis CD, Setayesh RM. Hemorrhaging associated with endosseous implant placement in the anterior mandible: a review of the literature. J Periodontol 2004;75:631–45.